At age 9, Autumn had outgrown other beds. Diagnosed with Angelman Syndrome, sleep was a real challenge. She was also prone to wandering which made most of the typical bedding options on the market a real challenge. Autumn’s mother, Michelle Ozick said this affected not only Autumn but all family members’ ability to sleep as well. The solution from Medicaid: “just put a mattress on the floor.” Enter Anthony Paulis, who has been involved with Autumn for 6 years, Anthony, realized that this just wouldn’t work for Autumn when he saw The Safety Sleeper® from Abram’s Nation, he knew he had the solution. But he also had another problem: how to get Medicaid to step up and pay for the bed.
“I treated it like a war, because nobody gets a bed,” Anthony said. “I needed to bring as much ammunition to the battle as I could. They don’t want to give it to you, and unless you fight tooth and nail, you won’t win.”
Anthony is eager to share his story with other families, hoping his experience will help others navigate the complexities of Medicaid and insurance reimbursements, and connect more children with a safe place to sleep that supports their medical diagnoses.

The Basics
Anthony started where everyone does: identifying the need for The Safety Sleeper® with the help of Autumn’s team of social workers and therapists. Several resources provided a good place to start:
- Information from the Angelman Syndrome Foundation. Similar groups exist for other diagnoses, and staff from these organizations are a lifeline for families. Anthony spoke with ASF’s CEO Amanda Moore and Dr. Eric Wright from their family resources team. “Eric was very helpful,” Anthony said. “He helped me think about strategies to deal with the appeal process, the state and Medicaid, as well as paperwork. It helped me understand what to gather, including a letter of necessity, and recommendations and medical information from doctors, medical professionals, and specialists.”
- Information from Abram’s Nation. Anthony spent time speaking with several staff members about Autumn’s unique needs and how to best meet them.
- Information from his DME rep. Anthony connected with a DME representative, Justin, who helped him collect information about Autumn’s needs to submit the first request.
It came as no surprise when Anthony’s first request was declined. Anthony expected as much. But what was surprising was how hard it was to understand why his request had been denied. The paperwork he received was vague and included a lot of technical information like administrative codes but no context to understand what they meant. It wasn’t adding up. To win the appeal hearing, Anthony realized he needed to understand the grounds on which the case for appeal would be built.
Getting the Right Information
Confused by the codes in his denial letter, Anthony reached out to his DME representative, Justin Walker, from National Seating and Mobility, and that conversation produced his first big surprise.
“What nobody tells you is that what the state tells the DME is not what the state tells you. I asked to look at what the state sent them, and when I compared it to mine, I was like, ‘holy crap!’ The paperwork you get looks a lot different than what the DME gets. Our DME’s paperwork had details about administrative code, questions, and information was broken down. If they would have asked me those questions in plain English, I could have answered those questions a heck of lot sooner!”
Like Perry Mason, Anthony was able to use this information to dig in. He understood the grounds for the denial, and with that critical information he was able to build a case for an appeal to Medicaid. And that would mean going to court. Anthony says getting all your documentation from doctors, specialists, school teachers, therapists and more are needed.

Requesting the Appeal
Anthony wasted no time in writing the appeal. Documentation from the DME noted that the “Service Procedure Requested is not supported by submitted documentation.” Other details noted that Medicaid believed there were less restrictive options available and specifically focused on the use of a hospital bed, and they questioned referrals from behavioral and occupational therapists. These were the areas Anthony focused on to get more information.
By chance, he had also been pursuing an appointment with the specialists at The Angelman Syndrome Clinic at Rush University Medical Center. During the family’s visit the doctor agreed that The Safety Sleeper® offered a number of medically-necessary features that went far beyond what a hospital bed could offer for Autumn. Therapists and Neurologists provided letters with more details. The family also provided a narrative that addressed the issues, such as wandering and seizures, that made a hospital bed a dangerous choice. Anthony included facts from the CDC, and statistics about why a mattress placed on the floor was an unacceptable solution as well. “It is very important to have all the paperwork and all of the doctors your child has seen. This could include neurologists, doctors, physical therapists, and any other specialists,” Anthony says.
Based on the additional information provided, a judge decided to grant the appeal and hear the case.
The Court Date
Appeals are rare, and Anthony is the first to admit he wasn’t entirely sure what to prepare for. So, he prepared for everything.
One of the most important things, he says, was having members of Autumn’s support team involved. “I wanted to have the backup of a therapist in case there was something I couldn’t answer,” he said. “And I’m glad I did, because there was one question they were able to answer during the hearing that I couldn’t, and it really helped having the therapists (Dresden Warminski and Trevor Witta) from MKE Behavioral there for us in our time of need.
Preparation also helped when a letter with questions from Medicaid appeared the same day as the hearing, giving Anthony just two hours to respond to several questions. But he dug into his research and answered with a four-page singled-spaced document.
Being that COVID-19 was on the rise, the hearing happened virtually. After hearing from Anthony, and Autumn’s mother, Michelle Ozick, Autumn’s team of doctors, specialists, and therapists, and reviewing the information submitted, the judge ruled in Autumn’s favor and they won the appeal hearing.
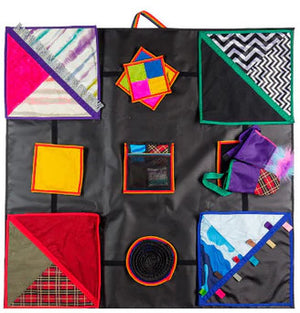
The Bed
While it did take a few months to process the order from Medicaid, Autumn’s bed arrived on March 31, 2021. The family’s dedicated DME, Justin Walker, was on site to help set up The Safety Sleeper® for Autumn.
“The Safety Sleeper® has been a godsend,” says Anthony. “Autumn loves her Safety Sleeper bed; she stays in it and doesn’t want to leave. That’s her chill spot, she’s there most of the time. It’s not just a place to sleep, and I can’t even describe how good it’s been for her!”